Injection Overmolding for Aesthetics and Strength Part 1
Orthodontics has seen significant advances during the past decade. In spite of these advances, there is no magic wand or silver bullet when teeth are undersized. In addition, there are a staggering number of adult ortho cases that produce the dreaded black triangle, an aesthetic dilemma that is considered to be more unsightly than the crowding that led to the ortho in the first place. Part one of this 2-part article will discuss the treatment of undersized teeth, and part 2 will discuss post-ortho black triangles.
Fracture Resistant Restorative Dentistry
In 1890, G. V. Black proposed both a cavity classification system and cavity preparations that remain intact and the standard of care 120 years later. The consummate scientist that was G. V. Black, we can assume, would be shocked to find today we still cling to both of his systems in spite of advances in almost everything: photoelastic studies in stress and strain, modern engineering, adhesive materials, magnification, outcome studies, the epidemic of cracked teeth, computers, the telephone, and the list goes on and on.
Restorative Papilla Regeneration
When a clinician faces the difficult challenge of papilla regeneration, there are many options available. In this article, I present a feature case that includes restorative treatment followed by papilla regeneration; a discussion of the pertinent literature is included. This case explores a cost-effective, minimally traumatic, and predictable approach. I then briefly review other traditional treatment modalities that are available to resolve this clinical dilemma, including orthodontic treatment or re-treatment, prosthetic intervention, and microsurgical papilla-regeneration procedure.
Bioclear Veneers vs Porcelain Veneers
https://www.youtube.com/watch?v=G1Al6K4q_CA
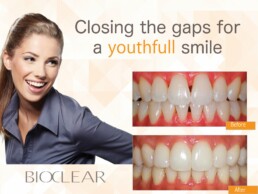
How does Bioclear differ from porcelain crowns and porcelain veneers? Well, porcelain dental crowns and veneers have been the default solution offered by cosmetic dentists to correct minor imperfections in teeth ranging from breaks, chips and gaps to decay, slight overlaps and discoloration. The veneers are just thin porcelain shells placed in the front of the aforementioned damage to leave smiles symmetrical and teeth bright and free of those stains, breaks, chips or gaps. They can wind up looking great, but securely bonding them to teeth always involves making space for them by removing a layer of healthy tooth enamel. In other words the dentist has to grind away some of an already damaged tooth to repair it with porcelain crowns or veneers.
So the process is not only permanent, it’s both comparatively time consuming and expensive. Fitting porcelain veneers typically requires at least two office visits over two weeks and costs between $1000 and $2000 per veneer. By way of contrast, no tooth enamel needs to be removed to place Bioclear veneers around damaged teeth. The injection-molding process used to fit them is completely reversible. It can be completed in a single office visit and it typically cost 25% to 50% less than traditional porcelain veneers. Moreover, while both varieties of veneer can be expected to have about the same ten year lifespan, Bioclear veneers are easier and therefore cheaper to replace or repair—in the event of damage—simply because they are easier for a dentist to remove. That means, with Bioclear patients can get all the benefits of porcelain crowns or porcelain veneers, without suffering the downsides.
Composite Versus Porcelain Part 3
Injection overmolding of teeth using the Bioclear Method invented by Dr. David Clark DDS has changed the way cosmetic dentists do composite restorations, and more importantly changing the way that we think about restorative dentistry. This is the second in a 3-part article series. You can find Part One Here and Part Two Here.
Composite Versus Porcelain Part 2
Injection overmolding of teeth using the Bioclear Method has changed the way cosmetic dentists do composite restorations, and more importantly changing the way that we think about restorative dentistry. This is the second in a 3-part article series. You can find part one here.
Repairing Jess' Broken Tooth
https://youtu.be/XtugPqU63K4
Jess contacted Tacoma, Washington’s Bioclear Dental Clinic after having had an unfortunate accident. She’d broken two teeth, a front tooth and the tooth next to it. Fortunately, her other front tooth was completely undamaged. So Dr Clark's primary cosmetic challenge, as he endeavored to restore her smile and repair her broken teeth, using The Bioclear Method, was simply color matching the composite resin to the intact tooth. Give the video a watch and let us know what you think of the results.
Composite Versus Ceramics Part 1
Injection overmolding of teeth using the Bioclear Method is changing the way that we do composite restorations, and more importantly changing the way that we think about restorative dentistry.
A Microscope for Every Dentist
Magnification, Advanced Magnification, Extreme Magnification. What does that mean to a general dentist? To help explain lets explore the parallel continuum of magnification and computer processing power. However, because powers of magnification have a squared, not linear relationship to visual information, a seemingly small jump in magnification creates a level of visual information that will profoundly impact the potential for clinical accuracy
How Bioclear Can Work for You
If your smile has imperfections … Gaps, chips or discoloring that you hide when your picture’s snapped? It doesn’t have to. The Bioclear Method developed by Dr. David Clark can improve the shape, size and fit of your teeth. Bioclear is an innovative alternative to traditional dental crowns and porcelain veneers. It’s an ideal restorative option for perfecting smiles. By utilizing the Bioclear Method cosmetic dentists can repair a tooth or redesign a smile by encapsulating teeth in dental composite with little or no drilling. Said composite can then be injection molded around a decaying, worn or damaged tooth in patented ultra-thin clear shapes (The Bioclear Matrix) that slide easily between the teeth and between the tooth and gums. That means it won’t require the dentist to grind away some of your tooth the way getting porcelain crowns or veneers would’ve.